The Role of Gut Microbiota in Autoimmune Diseases
1. Introduction
The human gut microbiota—a complex ecosystem of trillions of microorganisms residing in the digestive tract—plays a crucial role in maintaining overall health. Recently, research has linked imbalances in gut microbiota, or dysbiosis, to a range of autoimmune diseases, where the immune system mistakenly attacks the body's own tissues. Conditions such as rheumatoid arthritis, multiple sclerosis, and inflammatory bowel disease have shown associations with specific alterations in gut microbiota composition (Finckh et al., 2022). This review evaluates emerging evidence on the gut microbiota's role in autoimmune diseases, examining potential mechanisms through which microbial imbalances may contribute to immune dysfunction and discussing prospects for microbiome-based therapies.
2. Critical Review
2.1. Gut Microbiota and Immune System Interaction
The gut microbiota plays a fundamental role in immune regulation, with microbial communities interacting closely with the immune system to maintain a balanced immune response. Regulatory T cells (Tregs), crucial for preventing autoimmunity, are influenced by specific gut bacteria such as Bacteroides fragilis. These microbes produce short-chain fatty acids (SCFAs), which strengthen the gut barrier and reduce inflammation (Zhang et al., 2023). Dysbiosis, or a disturbance in microbial balance, can lead to reduced Treg activity and increased inflammation, creating conditions that may trigger or worsen autoimmune diseases.
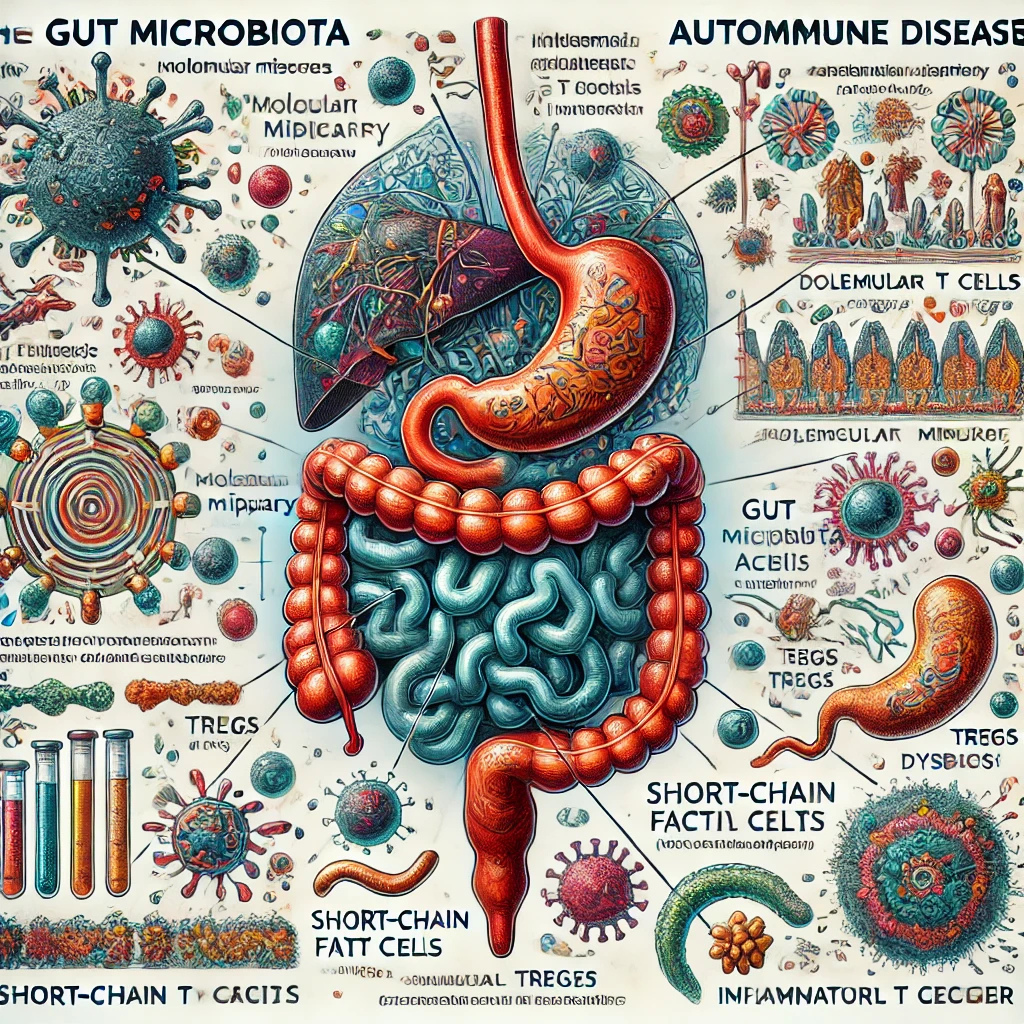
Another key component is molecular mimicry, where microbial antigens resemble human proteins closely enough that immune cells may mistakenly attack the body’s tissues. For example, gut bacteria linked to rheumatoid arthritis, such as Prevotella copri, can provoke an immune response that resembles autoantibody production, leading to joint inflammation. These findings underscore the intricate connection between the gut microbiota and immune regulation, highlighting its relevance in autoimmune disorders (Goswami et al., 2022).
3. Emerging Evidence in Autoimmune Diseases
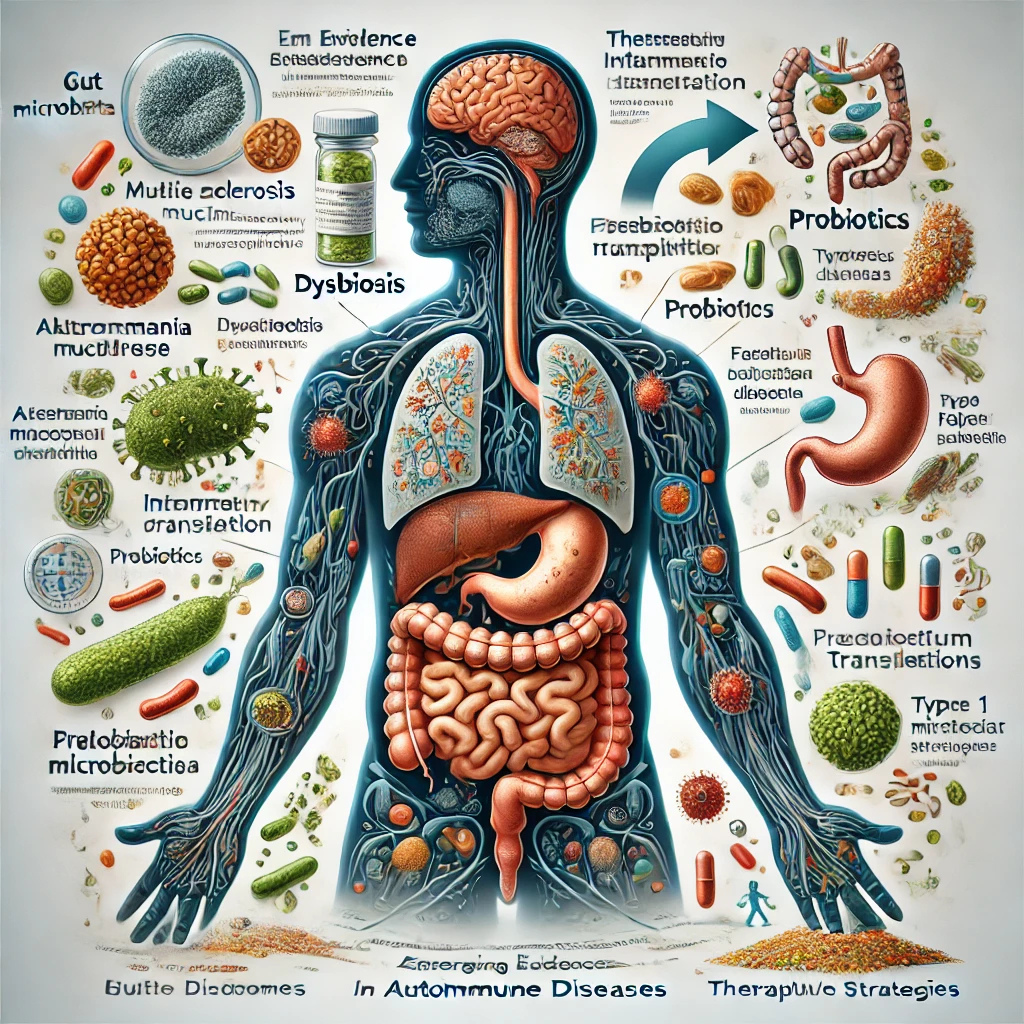
Studies have provided compelling evidence for the gut microbiota’s role in autoimmune diseases. In multiple sclerosis (MS), researchers have identified that MS patients often exhibit a higher prevalence of pro-inflammatory gut bacteria like Akkermansia muciniphila, which can exacerbate neuroinflammation. In contrast, beneficial bacteria that promote anti-inflammatory responses, such as Faecalibacterium prausnitzii, are typically reduced in MS patients. Experimental studies in animal models have further demonstrated that transferring dysbiotic microbiota from MS patients into healthy mice induces autoimmune-like symptoms, supporting a causal relationship.
Inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, has been strongly associated with gut microbiota imbalances (Adolph et al., 2022). Research has shown that patients with IBD often have reduced levels of beneficial bacteria and an increased abundance of pathogens. Fecal microbiota transplantation (FMT) trials, where gut bacteria from healthy donors are introduced into IBD patients, have shown promise in restoring microbial balance and reducing inflammation.
In type 1 diabetes, a condition where the immune system attacks insulin-producing cells, studies have indicated that lower diversity in gut bacteria during infancy may increase the risk of developing the disease later in life. Specific bacteria may play a role in educating the immune system early on, which, if disrupted, might lead to immune dysregulation. These examples illustrate how dysbiosis could contribute to autoimmune disease pathogenesis, with further research potentially uncovering microbial targets for therapeutic intervention.
4. Therapeutic Implications and Future Directions
Therapies targeting the gut microbiota offer a new frontier in autoimmune disease management. Probiotics, prebiotics, and fecal microbiota transplantation (FMT) represent potential strategies for restoring microbial balance and improving patient outcomes (Porcari et al., 2023). For example, probiotics containing Lactobacillus and Bifidobacterium strains are being studied for their anti-inflammatory properties in autoimmune disorders. While these therapies show promise, challenges remain, such as identifying specific microbial profiles that correlate with particular autoimmune diseases. Future research will be crucial in refining these approaches and developing individualized microbiome-based treatments, ultimately offering a potential pathway to mitigate or even prevent autoimmune conditions.
5. Conclusion
Emerging evidence underscores the significant influence of gut microbiota on autoimmune disease development and progression. By regulating immune responses, maintaining the integrity of the gut barrier, and preventing inflammation, a healthy microbiome appears essential for immune homeostasis. While therapies targeting the microbiome hold potential, more research is necessary to fully understand these relationships and translate findings into clinical treatments. As research progresses, the prospect of microbiome-based interventions could revolutionize the management of autoimmune diseases, offering hope for improved quality of life for affected individuals and potentially reducing disease incidence in the future.
6. References
- Finckh, A., et al. (2022). Global epidemiology of rheumatoid arthritis. Nature Reviews Rheumatology, 18(10), 591-602. Read More
- Zhang, D., et al. (2023). Short-chain fatty acids in diseases. Cell Communication and Signaling, 21(1), 212. Read More
- Goswami, T. K., et al. (2022). Regulatory T cells (Tregs) and their therapeutic potential against autoimmune disorders. Human Vaccines & Immunotherapeutics, 18(1), 2035117. Read More
- Adolph, T. E., et al. (2022). The metabolic nature of inflammatory bowel diseases. Nature Reviews Gastroenterology & Hepatology, 19(12), 753-767. Read More
- Porcari, S., et al. (2023). Key determinants of success in fecal microbiota transplantation. Cell Host & Microbe, 31(5), 712-733. Read More